International Journal of Clinical Case Reports 2016, Vol.6, No.21, 1-5
3
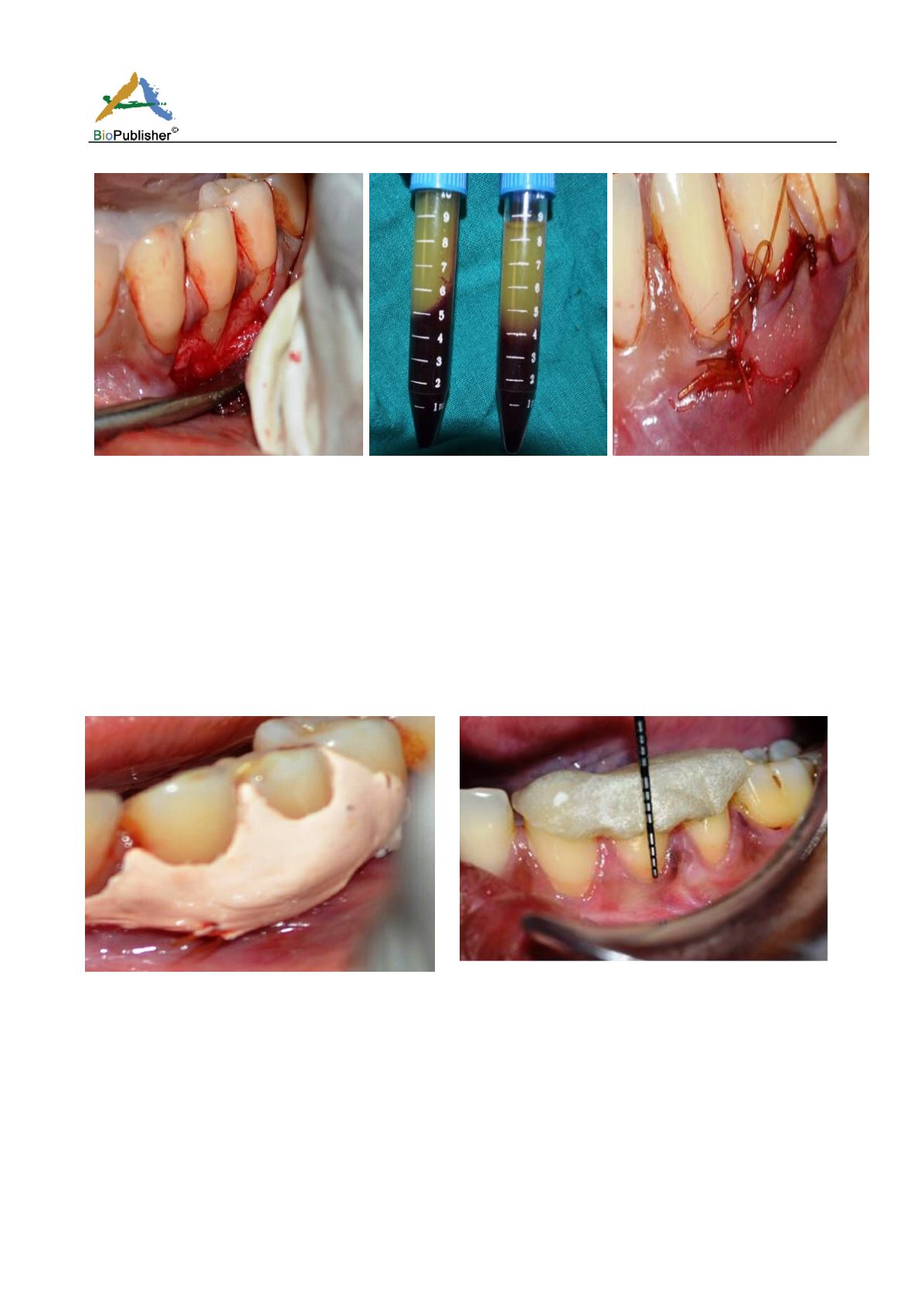
Fig.3 Full thickness flap elevated to
expose 3mm of the marginal bone
apical to the dehiscence area
Fig.4 Centrifuged blood consisting
of
three layers: Top most layer consisting of
acellular PPP; PRF clot in the middle;
and RBCs at the bottom
Fig.5 PRF clot placed over the denuded
root surfaces with the flap coronally
advanced and suture
Post-operative care: The patient was advised to use 0.2% chlorhexidine digluconate mouthrinse. Systemic
antibiotics were prescribed and the patient was advised to follow routine post-operative periodontal instructions.
Two weeks post-operatively dressing was removed and saline irrigation was done. The patient was monitored at
regular intervals and was kept under maintenance therapy. At the end of 1 month, clinical examination was done
(Fig.7). The recession defects showed signs of satisfactory healing and root coverage was accomplished without
any post-operative complication.
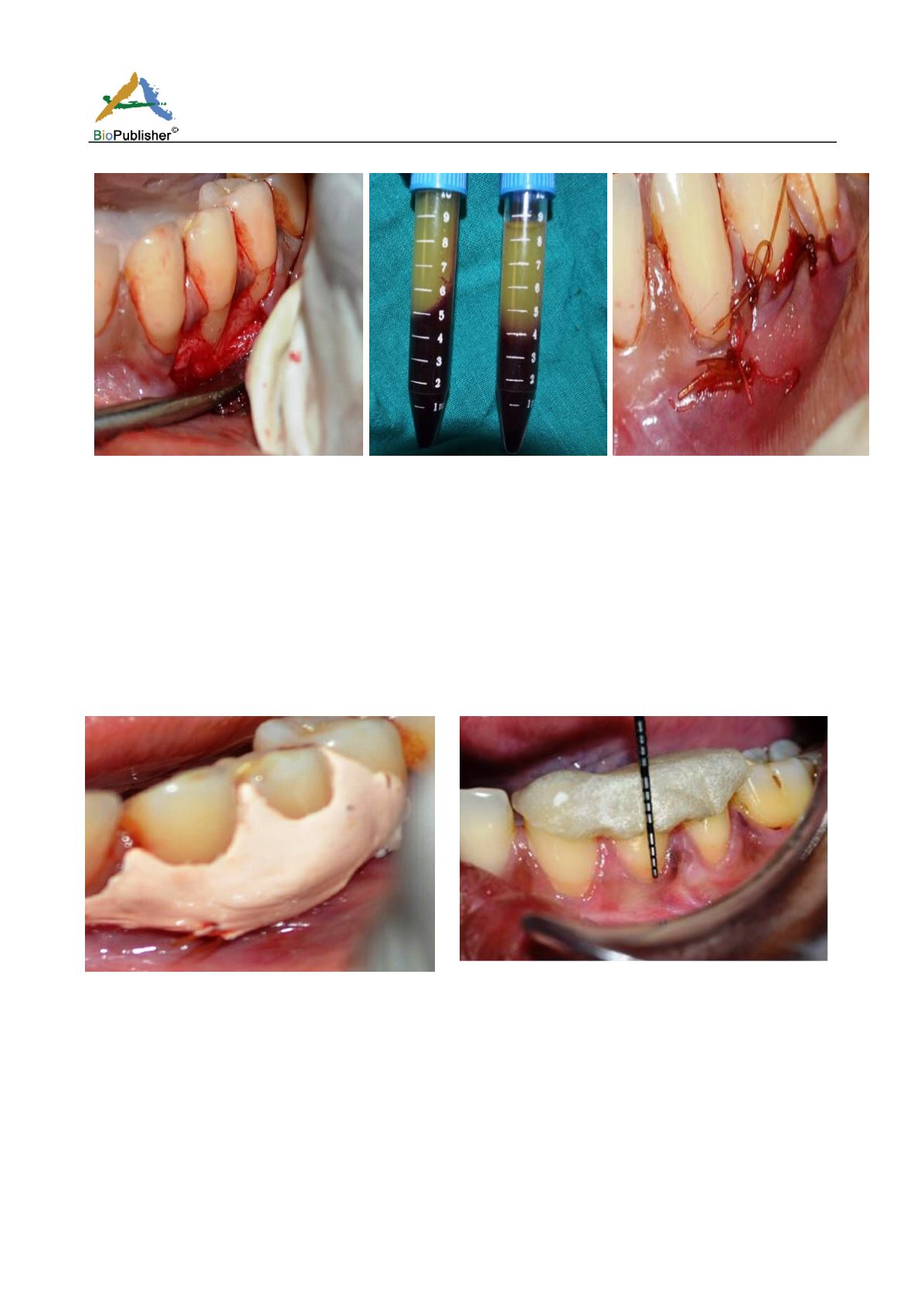
Fig.6: Periodontal dressing placed over the surgical area
Fig.7: Post-op clinical photograph at the end of 1 month with the
recession defects revealing signs of healing and root coverage
accomplished without any post-operative complication
Discussion
The ultimate goal of muco-gingival plastic surgery is aesthetic root coverage. Any therapeutic intervention aimed
at root coverage should be to restore the tissue margin at the cemento-enamel junction and to achieve an
attachment of the tissues to the root surface so that a normal healthy gingival sulcus with no bleeding on probing
and a minimal probing depth is present (Gupta et al., 2006). Various surgical procedures have been described to
treat gingival recessions, but these have been demonstrated to heal with a long junctional epithelium, and
regeneration has been observed only in the most apical portions of the lesion. The coronally advanced flap
procedure has been demonstrated to be a reliable treatment modality with a predictable outcome for obtaining root