Cancer Genetics and Epigenetics 2017, Vol.5, No.5, 25-27
26
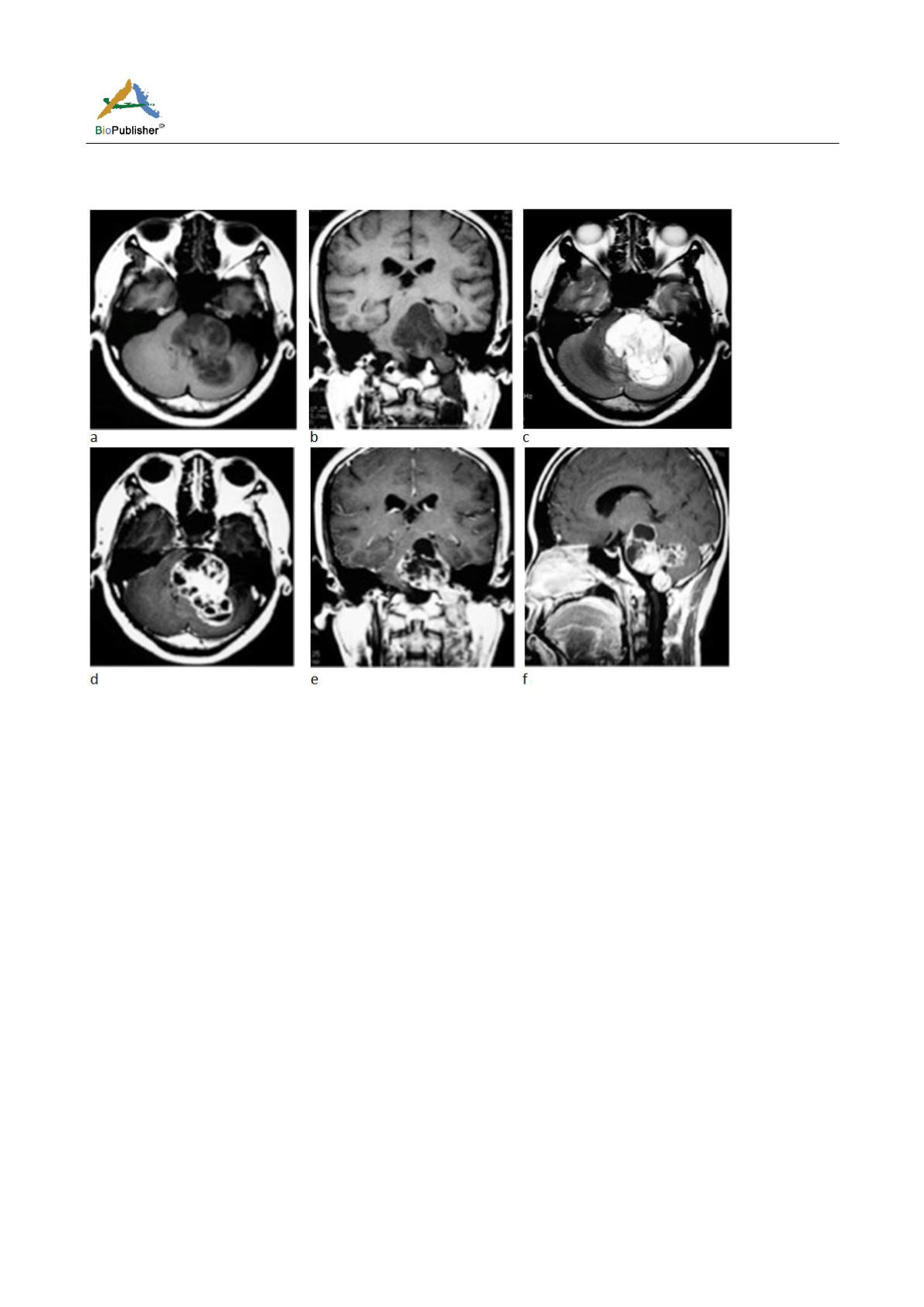
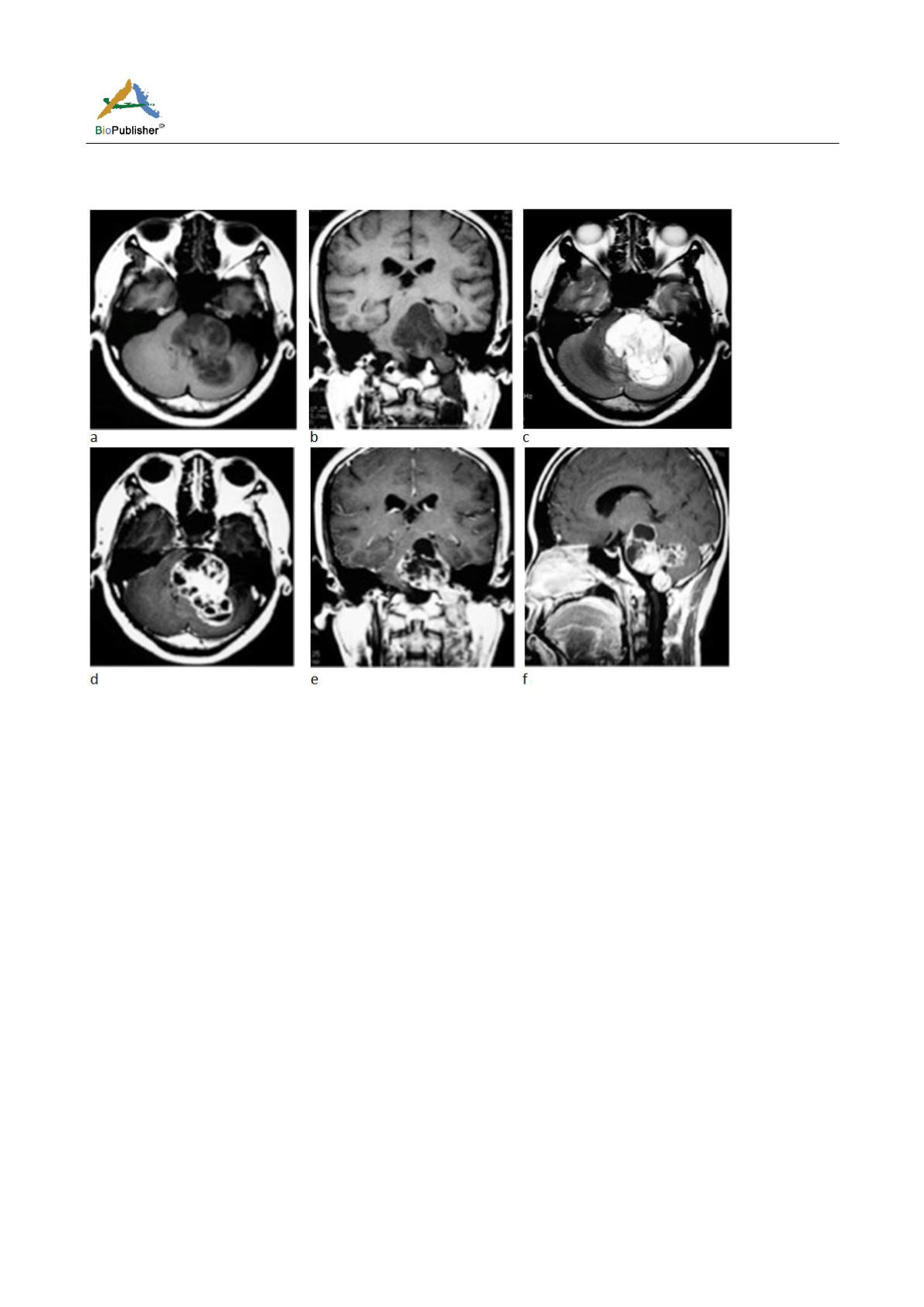
The individual nodules of the tumor were surrounded by a thin low-intensity capsule or septa on T2 weighted
images. No perilesional edema was noted. The fourth ventricle was compressed and shifted to the right upper side.
Figure 1 (a-f) MRI images showed a solid-cystic mass with multinodular appearance in the left CPA region
Note: Cyst compartments presented with slight hyperintense signal compared with cerebral spinal fluid (CSF) on T2-weighted
images; and solid compartments showed slight hyper signal intensity on T2-weighted and FLAIR images compared with parenchyma.
Contrast-enhanced T1-weighted images showed heterogeneous enhancement. The individual nodules of the tumor were surrounded
by a thin low-intensity capsule or septa on T2 weighted images. No perilesional edema was noted. The fourth ventricle was
compressed and shifted to the right upper side
2 Disscussion
Plexiform schwannomas have been reported to represent 4.3 % of all schwannomas (Nagata et al., 2015). Studies
have reported approximately 23% of all PSs arise in the head and neck region (Ijichi et al., 2017). While PS
located in the head and neck have been reported in literature, none of the reported tumors were presented in the
CPA space.
Clinically, schwannoma is seen commonly in adults of the age group ranging from 10 to 40 years with female
predilection of 2:11 (Lambade et al., 2013). Our case showed the same features to the literatures. The symptoms
of our case were related to the site of the tumor showing nonspecific features.
The most unusual feature in our case was the site, i.e. involvement of the CPA which has not been documented as
a location up to now. Consider the site of our case, an assumption that the association with posterior fossa nerve
can be made, although the nerve was not identified at the time of MRI scan. A solid-cystic mass, with intense
enhancement of the solid compartment, was detected around the fourth ventricle area pre-operatively. The lesion
was seen extending into the left CPA region. Since the tumor in our patient appeared to be originating from the
fourth ventricle, its diagnosis including ependymomas, followed by choroid plexus papillomas and
medulloblastomas were considered. In general, the latter two tumors contain more solid compartment. The
multi-cystic pattern and its location, therefore, provide very valuable imaging indicators of ependymomas.
Retrospectively, we repeated analysis of the pre-operative MRI images of the tumor. Virtually, the tumor was
growing around the fourth ventricle, rather than from the ventricle. By looking it over, the fourth ventricle was