International Journal of Clinical Case Reports 2015, Vol.5, No. 43, 1-4
3
Figure 7 revealing the surgically excised lesion
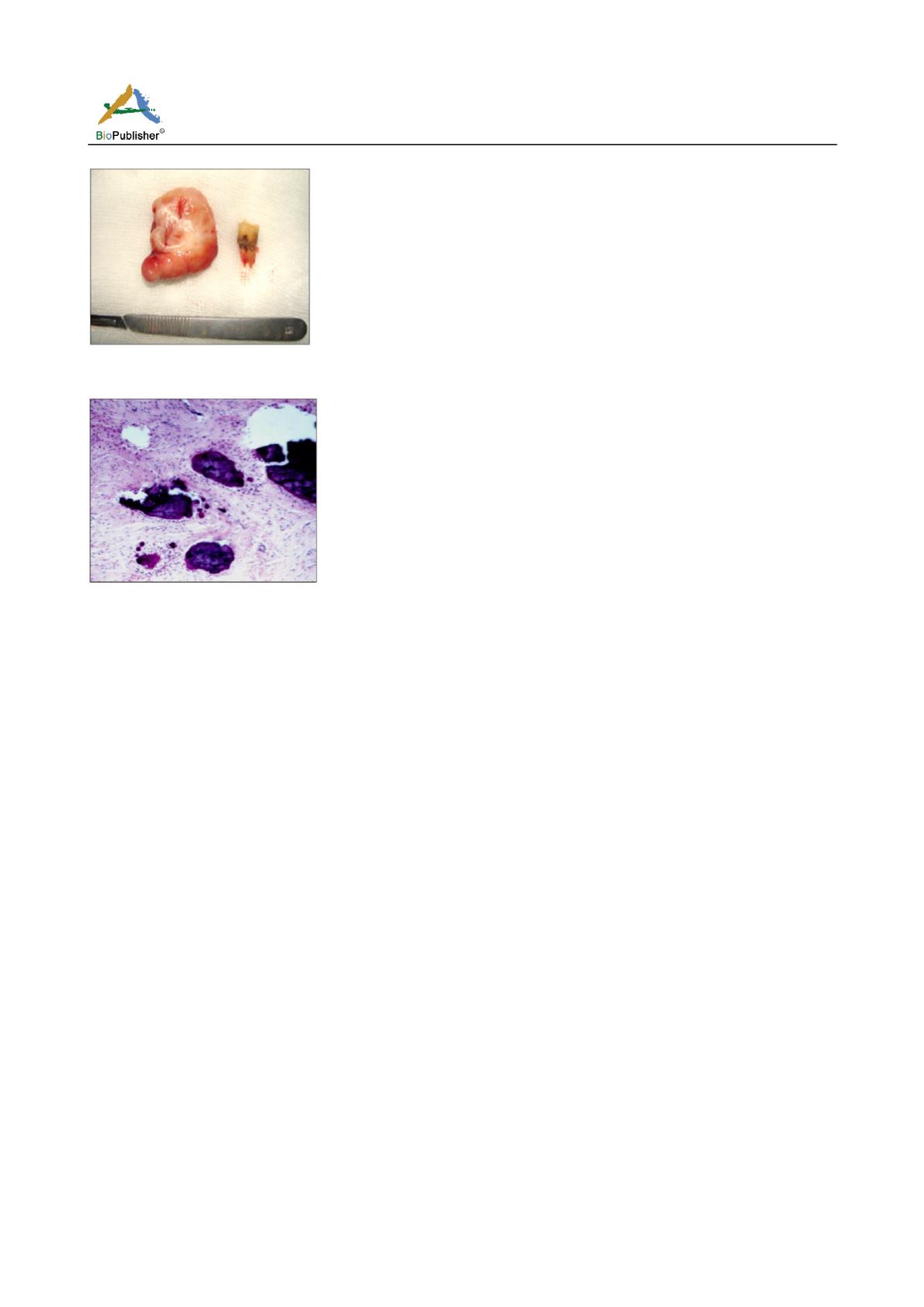
Figure 8 revealing the histopathological picture of the lesion
with parakeratinized stratified squamous epithelium with blunt
rete-ridges and with fibrous connective tissue stroma with
irregular osteoid containing osteocytes and osteoblasts
Discussion
Peripheral ossifying fibroma (POF) is a common
solitary gingival growth thought to arise from the
periodontal ligament (Jain and Deepa, 2010). The
commonly used synonyms for POF include peripheral
cementifying fibroma, peripheral fibroma with
cementogenesis, peripheral fibroma with osteogenesis,
peripheral fibroma with calcification, calcifying or
ossifying fibrous epulis and calcifying fibroblastic
granuloma (Singh et al., 2010). Bhasker et al. in 1984
described this lesion as peripheral fibroma with
calcification while the term POF was coined by
Eversol and Robin (Mesquita et al., 1998; Keluskar et
al., 2008). The aetiology and pathogenesis of POF
remains unknown. Some investigators consider it a
neoplastic process, while others argue it to be a
reactive phenomenon; in either case, the lesion is
thought to arise from cells in the periodontal ligament.
Trauma or local irritants, such as dental plaque,
calculus, microorganisms, masticatory forces, ill-fitting
dentures and poor quality restorations have been
implicated in the aetiology of POF (Mesquita et al.,
1998; Singh et al., 2010). Chronic irritation of
periosteal and periodontal membrane is thought to
lead to metaplastic changes in the connective tissue
initiating the formation of bone or dystrophic
calcifications (Kendrick and Waggoner, 1996).Hormonal
influences may also play a role, given the higher
incidence of POF among females (Kenney et al.,
1989). The peripheral ossifying fibroma (POF) is a
common gingival growth usually arising from the
interdental papilla. Females are more commonly
affected than males (5:1) (Nazareth et al., 2011). The
lesion occurs in any age group, predominating in the
second decade of life and with a declining incidence
after the third decade. Only 0.5% cases are reported in
the older age group, (Keluskar et al., 2008) as in our
case POF occurred in a 60 year old male.
Approximately 60% of POFs occur in the maxilla and
they are found more often in anterior region,
(Farquhar et al., 2008)
the lesion in the present case
was however present in mandibular posterior region.
POF usually measures <1.5 cm in diameter and rarely
reaches more than 3 cm, but patients with lesions of 6
cm and 9 cm diameter have also been reported (Singh
et al., 2010). The growth in the above case was
significantly larger in size than the average lesion.
Basically, the lesion represents varying stages of a
fibroma with ossification as the name POF implies;
however, ossification or calcification may not be
evident in all cases, particularly in the earlier stages of
the lesion. POF can produce a mild cupping defect of
adjacent alveolar bone. Though radiographic changes
are not always seen with POF, occasionally foci of
radiopaque material may be seen; particularly in larger
lesions (Kumar et al., 2009) The present case
demonstrated marked dystrophic calcification within
the lesion
(Figure 4). Clinical findings alone are not
sufficient for a diagnosis of POF because there are
other conditions that may have similar clinical
appearances and clinical course, such as pyogenic
granuloma or peripheral giant cell granuloma. Therefore,
biopsy and histopathological examination is required
for a definitive diagnosis (Singh et al., 2010).
Histologically, POF appears to be a non-encapsulated
mass of cellular fibroblastic connective tissue of
mesenchymal origin with central areas of calcification
covered with a stratified squamous epithelium, which
gets ulcerated in 23%-66% of cases. Mineralization
can vary between cementum-like material, bone
(woven and lamellar) and dystrophic calcification