International Journal of Clinical Case Reports 2015, Vol.5, No. 34, 1-5
2
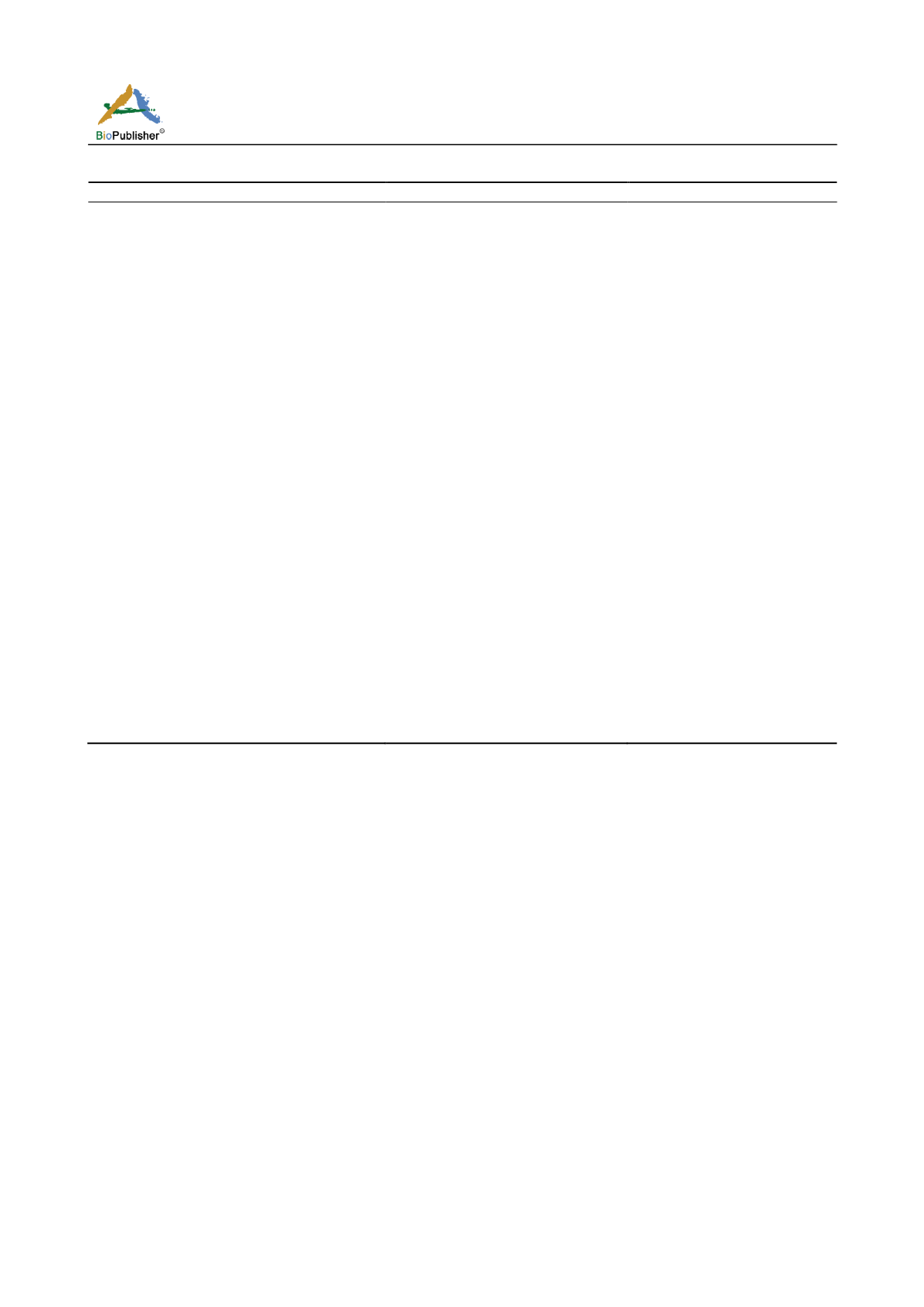
Table 1 Clinical assessment of swallowing ability using a thick liquid and puree
Before NMES+ST
After NMES+ST
Preparatory phase
Initiation
Labial closure
Jaw movement
Mouth opening
Bolus formation
Residual food on tongue
Residual food on hard palate
Residual food in buccal cavities
Normal
Intact
Intact
Normal
Inadequate
Yes
None
Yes
Normal
Intact
Intact
Normal
Good
None
None
None
Oral phase
Lingual function
Mastication
Oral transit time
Ability to maintain bolus
Tongue retraction
Food leaks/pushed out of mouth
Residual food in oral cavity
Number of swallows per bolus
Inadequate
None
Moderate delay (>3 s)
Inadequate
Inadequate
Yes
Yes
Double swallow
Intact
Inadequate
Intact (1 s)
Intact
Intact
Yes
No
Single swallow
Pharyngeal phase
Trigger swallowing reflex
Nasal regurgitation
Oral regurgitation
Laryngeal elevation
Force of laryngeal elevation
Wet voice after swallow
Cough after swallow
Respiration change after swallow
Fatigue
Delayed
No
No
Delayed
None
Yes
Yes
Yes
Yes
Normal
No
No
Normal
Inadequate
No
No
No
No
Water test
Failed
Passed
Abbreviations: NMES, neuromuscular electric stimulation; ST, swallowing training.
Previous studies have described the spontaneous relief
of neurologic complications within a few days to 1
month after surgical intervention (de Donato et al.,
2006; Biasi et al., 2008; Hanabusa et al., 2010). To
date, no study has provided recommendations for
therapeutic strategies effective in the management of
persistent dysphagia resulting from a giant ICAA after
surgical intervention. Our case provided a few clues as
to how the disease had manifested. Although there
was no definite major CN injury sustained during
surgery, the case was complicated by weakness of the
left vocal cord, resulting in hoarseness. This symptom
may have been caused by postoperative inflammation,
which is quickly relieved, according to previous
studies (Waespe et al., 1988; de Donato et al., 2006).
The severe persistent oropharyngeal dysphagia noted
in our patient may have been related to prolonged left
CN IX compression, discovered during the surgical
procedure. The finding of tongue deviation is also
suggestive of CN XII involvement. CN IX, part of CN
X, CN XI, and CN XII, as well as the jugular vein and
carotid artery, meet in the retrostyloid space (Waespe
et al., 1988). We assumed that the growing aneurysm
may have compressed, stretched, or induced ischemia
in the nerves in this area, resulting in dysfunction.
Our patient did not initially respond to ST; thus,
NMES and ST combination therapy was employed.
Burnett et al. (2003) reported that NMES may lower
the hyolaryngeal complex and provide resistance to
hyolaryngeal elevation; as such, it can be used for
muscle strengthening.
t al. (2007) demonstrated
in a prospective case study that NMES has positive
effects on cortical activation, cortical excitability, and
neural activation. In our case, electrodes were applied
on the right side of the neck, lateral to the midline, to
increase strength and awareness in her right (sound)
side. This was combined with posture regulation,