International Journal of Clinical Case Reports 2016, Vol.6, No.22, 1-8
6
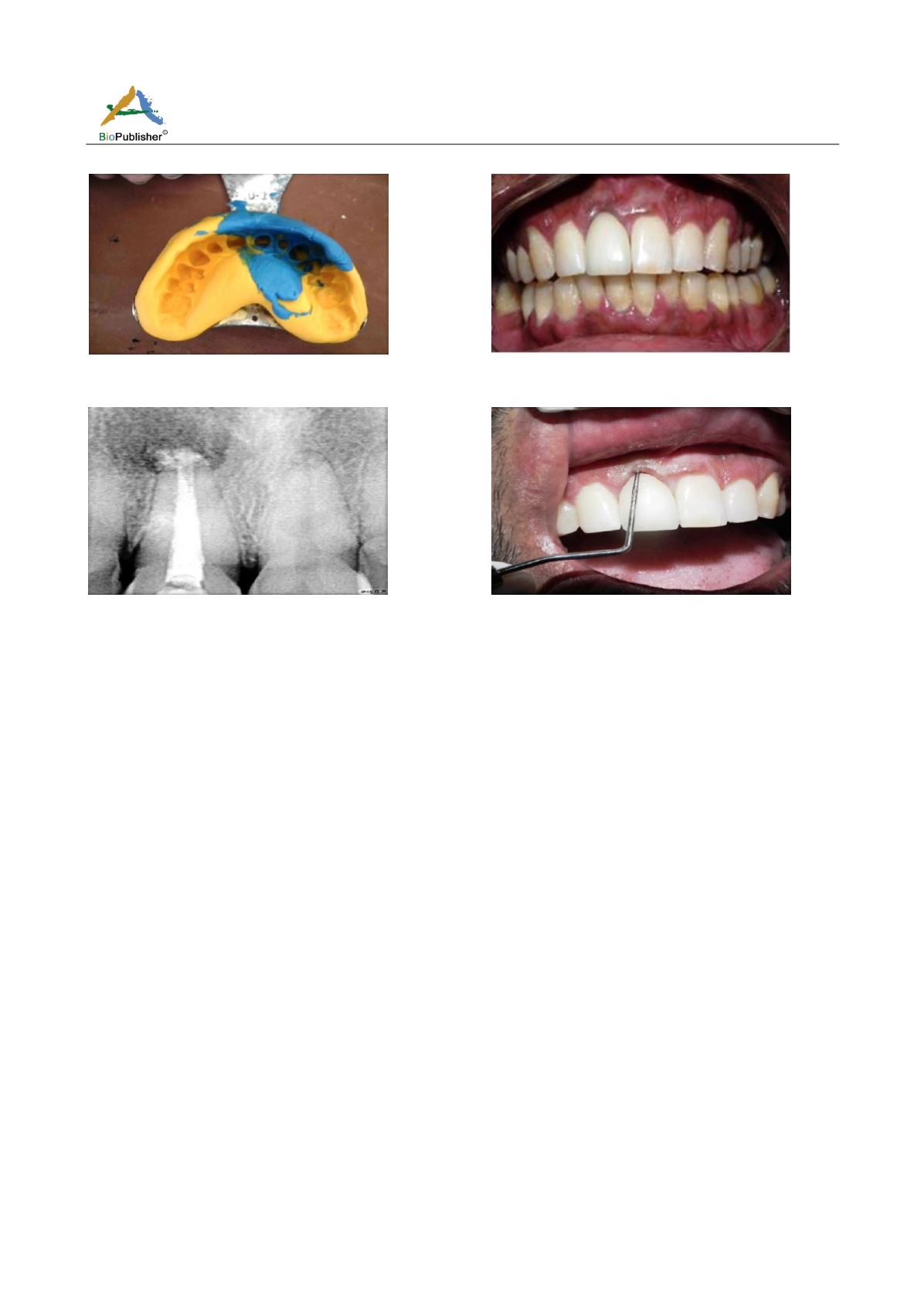
Figure 20 Showing elastomeric impression registered in
relation to 11
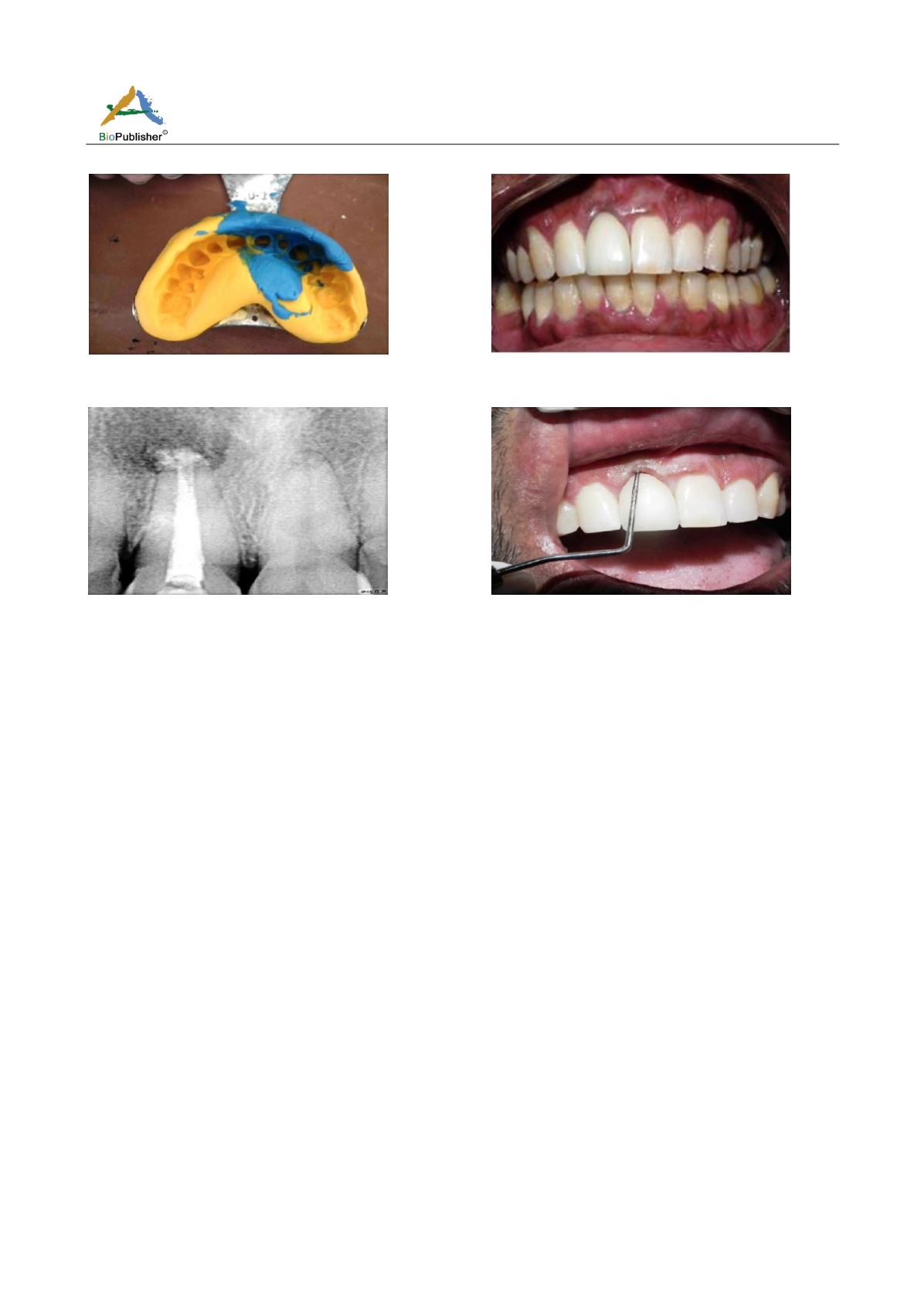
Figure 21 Showing all Ceramic Emax crown cemented in
relation to 11
Figure 22 Showing 12 months' post-operative radiograph
showing apparent bone fill with resolution of the osseous
defect
Figure 23 Showing pocket depth reduced from 15mm to
3mm
3 Discussion
The treatment of combined endo-perio lesions requires both endodontic therapy and periodontal regenerative
procedures, as discussed in the above case report. The goal of peri-apical surgical procedures is to remove all the
necrotic tissue from the peri-apical area to completely seal the pulp canal system to facilitate the regeneration of
hard and soft tissues including the formation of a new attachment apparatus (Karabucak and Setzer, 2009). Many
a times, there is no clear insult to the pulp noted in these types of lesions. The most common clinical/radiographic
features of these lesions include peri-apical radiolucencies and deep pocket depths associated with a non-vital
pulp. Traditional approaches to treat endo-perio lesions include non-surgical debridement of the root surfaces and
pulp canals, as well as surgical approaches that provide better access to clean the root surfaces and apical lesions
and to re-shape the surrounding bone/root apex. Bone loss caused by pulpal disease is reversible, whereas
advanced bone loss caused by periodontal disease is usually irreversible (Law and Beaumont, 2004). The
necessity of periodontal surgical therapy most likely remains because the periodontal bone loss is usually more
advanced and is less likely to resolve after non-surgical pulp canal therapy alone (Meng, 1999). Generally, partial
apical root resection has been suggested for all endodontic surgeries advised for extensive involvements
(Bashutski and Wang, 2009). In this case, we had planned a regeneration therapy for bone as well as the
periodontal ligament as it was supposed to lead to a better prognosis. Hence, we performed pulp canal
debridement with subsequent retrograde filling and removal of granulation tissue around the root apex.
Apicoectomy was done to prevent recurrence of infection as the maximum number of canal variations and
complexities are seen in the apical third (Siqueira et al., 1997). PRF i.e. Platelet rich fibrin, is in the form of a
platelet gel that is used in conjunction with bone grafts offering several advantages including promoting wound
healing, bone growth and maturation, graft stabilization, wound sealing and haemostasis, and improving the
handling properties of graft materials. It is saturated with growth factors which expediate the regenerative process
during healing (Choukroun et al., 2006). Also here, using the guided tissue regeneration (GTR) technique,
combined with bone graft, periodontal regeneration was clinically and radiographically evident after a 1-year
follow-up. The role of bone graft in the above case was to provide space for periodontal regeneration and for