International Journal of Clinical Case Reports 2017, Vol.7, No.13, 53-57
55
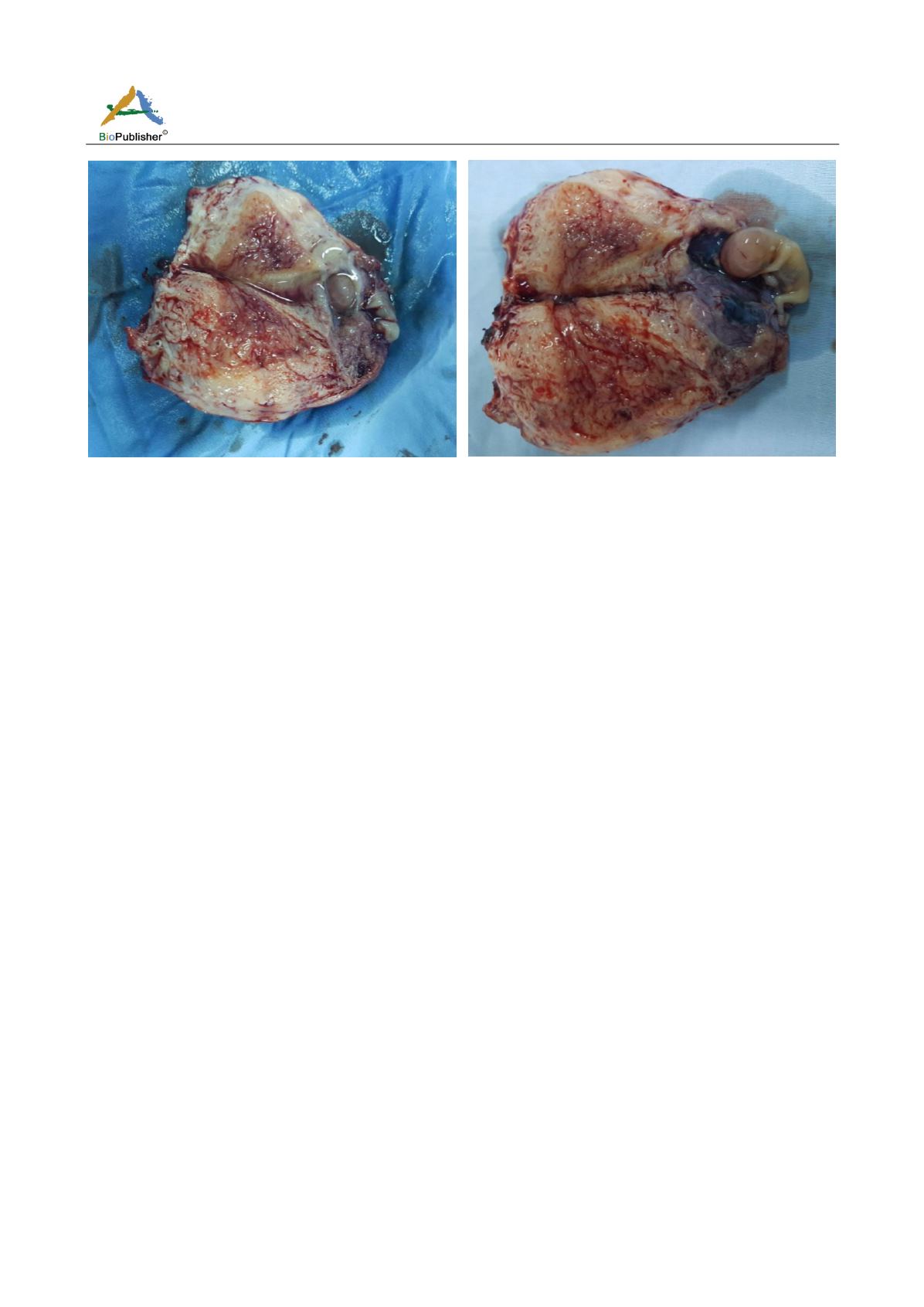
Figure 5
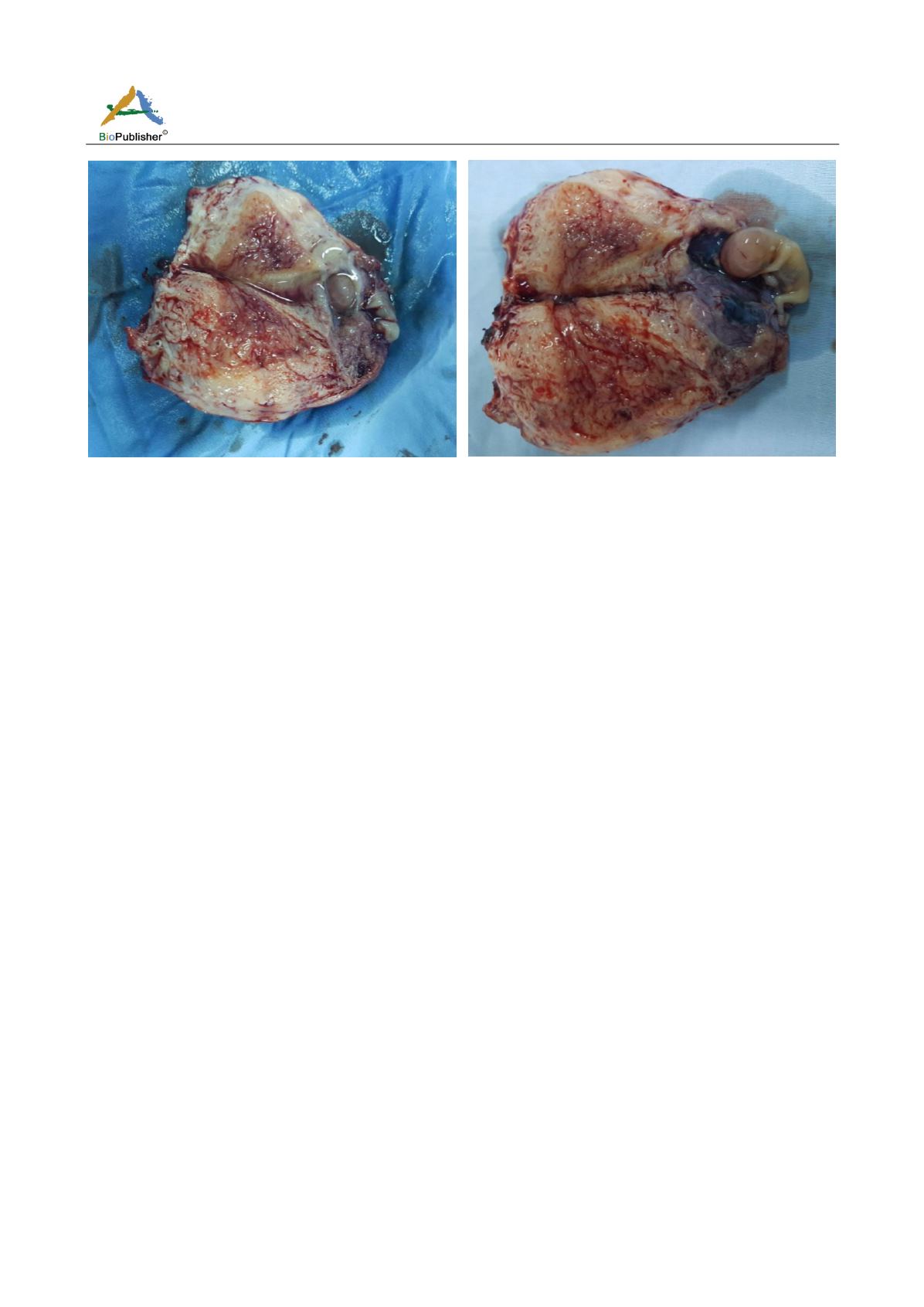
After opening the hysterectomy part the interstitial seat of the pregnancy is confirmed
The macroscopic examination of our hysterectomy part confirms well the interstitial seat of the pregnancy
(Figures).
The incidence of interstitial pregnancies is between 2-3% of all ectopic pregnancies and allows relatively late
development until 16 weeks of amenorrhea (11 weeks of amenorrhea for our case). Interstitial pregnancies are
particularly hemorrhagic due to a rich corneal vascularization and greater myometrial distension, so that the rate
of mortality by interstitial pregnancy is logically 2 to 3 times that of tubal pregnancies (Malek-mellouli et al.,
2012).
Risk factors are similar to other ectopic pregnancies (history of ectopic pregnancy, pathology and tubal surgery,
intra-uterine dystylbene exposure, genital infections, tobacco, in vitro fertilization) except for ipsilateral
salpingectomy which is a specific risk factor to interstitial pregnancy (Tulandi and Al-Jaroudi, 2004), in our
patient alone contraception by micro progestative was found as risk factor for ectopic pregnancy.
The diagnosis is based on synthesis of clinical examination, plasma HCG and transvaginal ultrasound.
The ultrasound diagnosis of interstitial pregnancies is difficult, and these pregnancies are often symptomatic later,
leading to delays in management until the second trimester, but ultrasound criteria have been proposed by
Timor-Tritsch for this diagnosis: An empty uterine cavity, an eccentric gestational sac and located at>1 cm from
the lateral wall of the uterine cavity and a thin (<5 mm) layer of myometrium around the sac (
Timor-Tritsch et al.,
1992
). 3D ultrasound as well as MRI also allow early accurate diagnosis if interstitial pregnancy is suspected on
2D ultrasound (Filhastre et al., 2005; Júnior et al., 2007).
In our case the diagnosis was delayed to 11 weeks of amenorrhea, the patient did not consult since she attributed
its disorders of the cycle to the contraceptive treatment, the ultrasound examination (Figures) confirmed the
diagnosis of cornual pregnancy, there is no 3D probe in our department and it was not considered useful to
perform an MRI since it was decided to perform a laparoscopy.
By the past, the treatment of interstitial pregnancy consisted of salpingectomy and corneal resection by
laparotomy, probably as a result of delayed diagnosis (Moawad et al., 2010) currently interstitial pregnancy is
typically diagnosed at an early gestational age and prior to rupture, leaving the opportunity for conservative
medical or surgical treatment (Hussein et al., 2014). However, in the presence of signs of severity (hemodynamic
failure and presence of abundant hemoperitoneum), the treatment should be surgical by laparoscopic route if
possible, but most often by laparotomy. Conservative treatment of the uterus will be preferred whenever possible,
but radical treatment (hysterectomy) may be necessary to control hemorrhage (Hussein et al., 2014).