International Journal of Clinical Case Reports 2015, Vol.5, No. 38, 1-3
2
Figure 1b Lateral view KUB of migrated IUCD
KUB showed Radiopaque IUCD is seen in superior
aspect of the pelvic cavity, below the left sacral alar.
Lateral abdominal x ray showed IUCD seen in
presacral space. Ultrasound both vaginal and abdominal
both failed to locate the IUD within the uterus. Patient
was very keen to have the IUCD removed as it was
causing her abdominal discomfort and also mental
discomfort having known of a dislocated foreign body.
Patient was aware of the risk including open surgery,
bladder and bowel injury including the need to resect
part of the bowel or bladder and stoma insertion.
Patient insisted to have the IUCD removed despite the
potential risks.
Diagnostic laparoscopy with pre-operative bowel
preparation and the possibility of laparotomy, colonoscopy,
bowel resection and or bladder repair was conducted
with the presence of the surgical team. Diagnostic lap
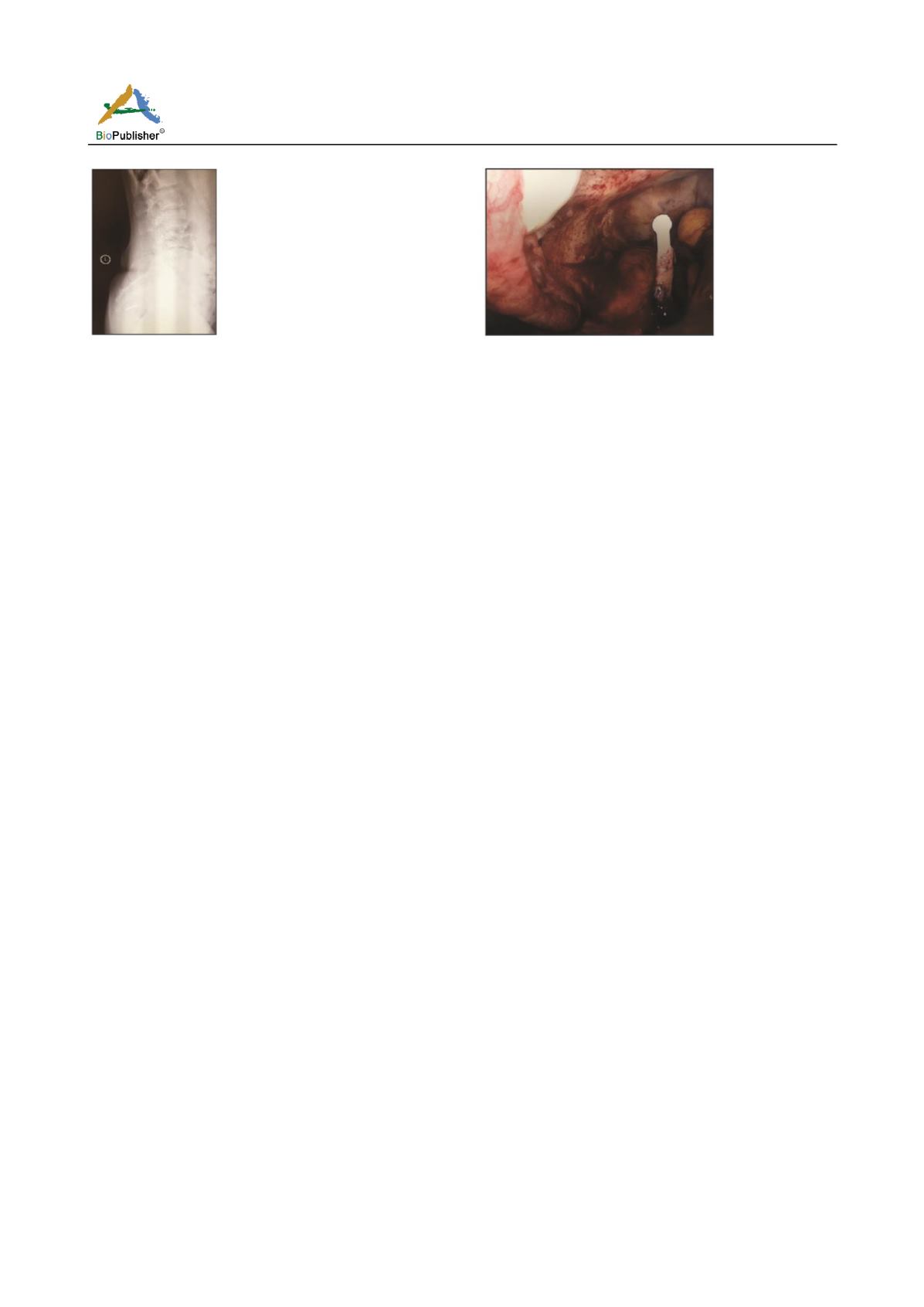
showed T shape IUCD over sigmoid colon with one
arm seen while the remaining of the IUCD appears to
be embedded within the rectum (Figure 2). Examination
under anaesthesia and colonscopy was done by surgical
team revealing a foreign body felt at 10 cm from anal
verge and on table sigmoidoscopy found full thickness
erosion of IUCD at 12 cm.
It was decided by the surgical team where she had an
anterior resection of the rectum, on table lavage and
primary anastomosis via a midline laparotomy. Patient
recovered well post operatively and sent home at day
7. Histopathology showed IUCD but no obvious
pathology. Follow up at one month, patient was well
with daily bowel opening. Both chest and abdominal x
rays were unremarkable. Further follow up at 3
months patient remained well and the case was closed.
Discussion
IUCD is safe and a commonly used long term method
of contraception. Associated complications include
Figure 2 Laparoscopic view of migrated IUCD
bleeding, infection, uterine perforation and subsequent
migration to adjacent organs which is the most severe
amongst all complications. The perforation is thought
to occur at the time of insertion or occur due to chronic
inflammatory reaction to the copper- containing foreign
object leading to gradual erosion through the uterine
wall (Darlong et al., 2009). Multiple reports of coil
migration has been reported including large bowel e.g.
rectosigmoidal region (Darlong et al., 2009), small
bowel (Oxby et al., 2006), appendix (Katara et al.,
2004), urinary bladder (Wei et al., 2003) and ureter
(Qublan and Dabbas, 2002) while a Cochrane review
confirmed the risk of such complications remains
similar regardless the type of copper coil used (Kulier
et al., 2007).
Although perforation may be suspected when patient
complain of pain or bleeding immediately after insertion,
a large proportion of cases remain asymptomatic even up
to 12 years after insertion (Mulayim et al., 2006).
Perforation and migration is usually suspected when
the IUCD string is no longer visible at the external os.
It is essential to diagnose the position of the IUCD
and consider its removal as malpositioned IUCD may
leads to pregnancy while migrated IUCD may cause
severe morbidity depending on the organ it migrated to. A
migrated IUCD towards the urinary bladder may stone
formation (Wei et al., 2003), while migrating to large
bowel such as sigmoid colon or rectum may lead to
symptoms such as adhesions, abdominal pain, bowel
obstruction, volvulus, bowel perforation or fistula
formation (Oxby et al., 2006; Mulayim et al., 2006).
First line diagnosis of a migrated IUCD should
include an ultrasound and abdominal x-ray. Physical
examination including a rectal examination may also
be of help, although IUCD migrated to the upper part
of the rectum and beyond may not be felt during rectal